Dysthymia Disorder: Severe persistent depressive disorder

What is dysthymia disorder?
Dysthymia disorder, commonly known as PDD (persistent depressive disorder), is a chronic mood illness characterized by a constant feeling of hopelessness, sadness, and low mood that lasts for at least two years.
People with dysthymia can experience symptoms such as sleep issues, lack of energy, overeating or poor appetite, low self-esteem, feelings of pessimism, and difficulty concentrating.
Although these symptoms might not be severe enough to qualify as a major depressive episode, they can still significantly affect functioning and daily life.
Dysthymia is a chronic depressive disorder that may gradually worsen over time and coexist with other mental health issues, including anxiety or substance addiction. Treatment for severe persistent depressive disorder might include psychotherapy, a combination of drugs, and lifestyle changes.
Common types of dysthymic disorder
Here are a few common types of dysthymic disorder:
Dysthymic disorder is a type of mood disorder characterized by persistent depressive symptoms, including low energy and an impaired ability to experience pleasure or satisfaction. In addition to having these “typical” symptoms, people with dysthymic disorder often have problems functioning at work or school, have trouble socializing, and face significant personal difficulties.
an inability to enjoy pleasure and anhedonia. People with dysthymia may have trouble concentrating, frequent crying spells and a lack of interest in normal daily activities.
You may experience feelings of sadness, hopelessness, helplessness and irritability. Patients frequently have low energy, difficulty concentrating and sleeping well.
Dysthymic disorder with major depressive episodes
People with this type of dysthymic disorder experience both episodes of major depression and persistent low mood. It is referred to as “double depression” when a person with a dysthymic disorder has one or more significant depressive episodes.
In this situation, the person suffers from both the persistent low mood of dysthymia and the more acute symptoms of major depression. This depression might be particularly difficult to treat and may significantly affect a person’s regular functioning and quality of life.
Pure dysthymic disorder
The most typical dysthymic disorder is one in which a person has a persistently depressed mood without experiencing significant depressive episodes. Signs of PDD include decreased self-esteem, a lack of energy, issues concentrating, changes in sleep patterns and appetite, and feelings of pessimism or hopelessness.
The symptoms of PDD depression might be less severe than those of MDD (major depressive disorder). However, PDD is chronic and might significantly affect a person’s ability to work in daily life.
Late-onset dysthymic disorder
This kind of dysthymic disorder begins in adulthood and is commonly accompanied by a traumatic life event such as job loss or divorce. The late-onset dysthymic disorder generally refers to the onset of symptoms at 21 years of age or older.
Signs of dysthymic disease can include low self-esteem, poor appetite, oversleeping, and difficulty sleeping.
Besides, you may see other symptoms such as feelings of hopelessness, difficulty making decisions, poor concentration, or fatigue. This disorder might be challenging to diagnose because the symptoms can be long-lasting and mild. It’s crucial to recognize and treat this disorder.
It may impact a person’s quality of life and raise their chance of having a major depressive disorder.
Double depression
It is a kind of dysthymic disorder where a person experiences low mood and also has episodes of major depression. In this kind of depression, the person faces persistent feelings of hopelessness, sadness, and a lack of pleasure. You might stop enjoying things you used to like.
Double depression might be particularly difficult due to the chronic nature of dysthymia. It may make it challenging for the person to respond to the treatment. Treatment for double depression involves a mixture of drugs, psychotherapy, and lifestyle changes (healthy diet, exercise, etc.).
Early-onset dysthymic disorder
This particular dysthymic disorder starts in childhood or adolescence and lasts into adulthood. Early-onset dysthymic disorder (EODD) refers to cases where symptoms begin before age 21. Early-onset dysthymic disorder symptoms might be less severe than major depressive disorder symptoms.
Early-onset dysthymic disorder may continue longer. If you have EODD, you may also face episodes of major depression many times in your life.
What is MDD (major depressive disorder)?
MDD, commonly known as depression, is a mental health illness characterized by persistent feelings. It includes emptiness, sadness, and a loss of pleasure or interest in activities that were once enjoyable.
The symptoms of MDD might vary in duration and intensity, but they commonly last for at least two weeks or more and significantly interfere with regular life and functioning.
MDD is a severe condition that needs professional treatment. Treatment alternatives might include medication, psychotherapy, or a combination of both.
Persistent depressive disorder side effects
PDD symptoms might differ from person to person, but some of the most widespread signs and symptoms are as follows:
- Low fatigue and energy
- Changes in weight or appetite
- Persistent feelings of hopelessness or sadness
- Excessive sleepiness or insomnia
- Feelings of guilt or worthlessness
- Difficulty with social situations or relationships
- Suicidal behaviors or thoughts
- Physical symptoms include pain, digestive issues, and headaches.
- Loss of interest in activities or hobbies
- Issues in making decisions and concentration
Everyone’s experience with PDD is different, and a few people might not experience all these adverse reactions.
Persistent depressive disorder: drugs and treatment
Typically, a combination of drugs and psychotherapy is used to treat PDD. Here are a few common treatments and drugs used for PDD:
Treatments for PDD
Light Therapy:Light therapy exposes a patient to intense light for a set amount of time every day. It is generally used to treat SAD (seasonal affective disorder), but it is also effective in the treatment of severe persistent depressive disorder.
ECT (electroconvulsive therapy):ECT is a kind of therapy that involves sending electrical currents via the brain to prompt a seizure. If you haven’t seen any improvement in PDD from other treatments, you may try it.
Psychotherapy:Psychotherapy is a crucial part of the treatment of PDD. There are various types of therapy for PDD.
Types of Therapy for PDD
CBT (cognitive behavioral therapy)
CBT is well-known for treating depression, among other mental conditions. CBT focuses on changing negative behavior patterns and thoughts that cause depression. CBT may also help you:
- Learn relaxation techniques and coping skills.
- Explore how your behaviors, emotions, and thoughts impact your actions and life.
- Solve problems
CBASP
CBASP (cognitive behavioral analysis system of psychotherapy) is a newer therapy mainly developed for treating chronic depression. The motive of CBASP is to:
- Create social problem-solving skills.
- Grow empathy and interpersonal skills.
- Decrease isolation and improve functioning.
- Learn to recognize the effects of your behaviors.
Interpersonal therapy
IPT is a kind of talk therapy that focuses on social and relationship issues. It might contribute to the persistence of depression signs. IPT aims to improve your ability to communicate, address relationship problems, and deal with challenging emotions positively.
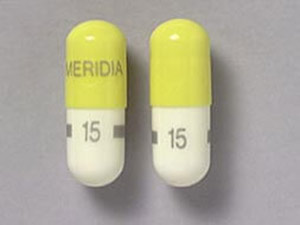
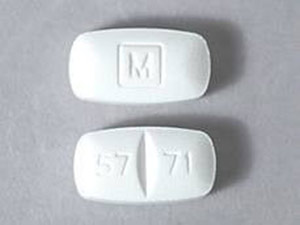
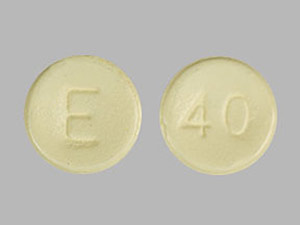
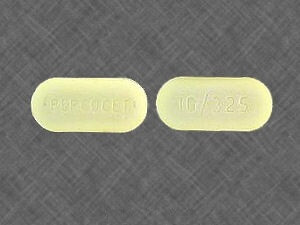
Drugs for persistent depressive disorder (PDD)
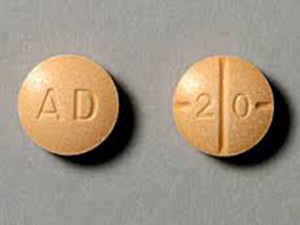
- Antidepressants: SSRIs (selective serotonin reuptake inhibitors), including fluoxetine or sertraline
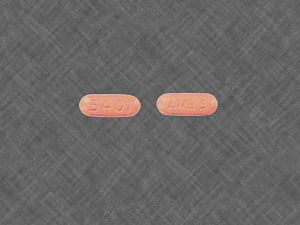
- SNRIs (serotonin-norepinephrine reuptake inhibitors), such as duloxetine or venlafaxine
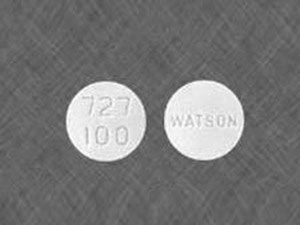
- TCAs (tricyclic antidepressants), including amitriptyline
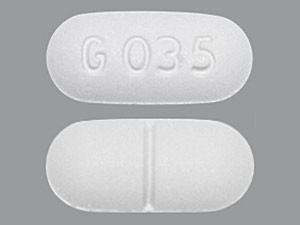
- Atypical antidepressants, such as Wellbutrin (bupropion),
What are the major differences between persistent and major depressive disorders?
PDD (persistent depressive disorder), also known as dysthymia, is a kind of depressive disorder that is characterized by a long-lasting, low-grade form of depression. whereas MDD (major depressive disorder) is a more acute form of depression characterized by the presence of one or more MDD episodes. There are a few major differences between MDD and PDD, such as:
Duration
The critical difference between MDD and PDD is the duration of the depressive symptoms. Persistent depressive disorder (PDD) is a chronic condition that lasts for at least two years, while MDD commonly lasts for a shorter period, typically a few weeks to various months.
Severity
While both MDD and PDD may cause significant impairment and distress, MDD is commonly more acute than PDD. The signs of MDD are commonly more intense and might interfere with a person’s ability to work in regular life.
Symptoms profile
Although the symptoms of MDD and PDD might overlap, there are a few differences in the symptom profiles of the two conditions. For instance, people with progressive depressive disorder might experience more chronic feelings of hopelessness and sadness, while people with MDD can experience worthlessness, suicidal ideation, and more intense feelings of guilt.
Recurrence
The major depressive disorder has a higher recurrence rate than the severe persistent depressive disorder. People who experience one episode of MDD (major depressive disorder) are at a greater risk of having another episode in the future.
In contrast, people with PDD might have ongoing symptoms but are less likely to face a distinct episode of depression.
Treatment
The treatment of MDD and PDD might involve similar interventions, like antidepressant drugs and psychotherapy. However, people with PDD might need longer-term treatment and more support to handle their ongoing symptoms.
Final takeaway
Hope! These details are essential to telling you about the persistent depressive disorder and major depressive disorder. The major depressive disorder causes severe, persistent feelings of hopelessness and other symptoms that make enjoying life challenging.
Persistent depressive disorder is a more chronic and lasting form of depression. Treatments and medicines are also mentioned in the above lines. If you have a persistent depressive disorder, you may try them to see the benefits.;